What is osteoporosis?
Osteoporosis is a disease that thins and weakens the bones. Bones become fragile and fracture (break) easily, especially the bones in the hip, spine, and wrist. In the United States, millions of people either already have osteoporosis or are at high risk due to low bone mass. Osteoporosis is a silent disease, meaning some people don’t know they have it until a bone is broken.[1]
How is osteoporosis diagnosed?
Osteoporosis is diagnosed by bone mineral density (BMD) of the spine or hip, which is measured with dual energy x-ray absorptiometry (DEXA) scans. A normal BMD is no more than 1 standard deviation (SD) below the average or reference value. Osteopenia (low bone mass) is 1-2.5 SDs below the reference and osteoporosis is 2.5 SD or more below the reference BMD value.[2]
What are some of the main medical treatments for osteoporosis?
The main goal of treating osteoporosis is to prevent fractures. This is done by strengthening the bones and by preventing falls. Medication treatments to strengthen the bones include bisphosphonates (alendronate, risedronate, etc.), raloxifene (Evista), calcitonin, and for more severe osteoporosis teriparatide (Forteo) and denosumab (Prolia).[2]
Have any supplements been studied for osteoporosis?
Many supplements have been studied for osteoporosis. Adequate calcium and vitamin D is important for preventing and treating osteoporosis, so if there’s not enough in the diet, a dietary supplement is recommended.[2] Other supplements such as multivitamins, vitamin K, and probiotics might also have some benefit, but higher quality research is needed.[3][4][5]
How could diet affect osteoporosis?
To keep bones strong and to prevent osteoporosis, a healthy diet sufficient in calcium and vitamin D is recommended.[2] A meta-analysis of observational research has found that Western diets involving fast food, refined foods, meats and sugar are associated with lower BMD in contrast to a Mediterranean diet pattern or dietary pattern higher in dairy.[6][7]
Are there any other treatments for osteoporosis?
One of the key goals of treating osteoporosis is to prevent fractures by preventing falls. Exercise that involves strength and balance training helps to prevent falls. Other recommendations which may reduce the risk of fractures include limiting alcohol and caffeine intake, stopping smoking, and increasing exposure to sunlight.[2]
What causes osteoporosis?
Anyone can develop osteoporosis, but it is more common in females of older age. Risk factors for getting osteoporosis include old age, low body weight, family history, smoking, certain medications (corticosteroids, anticonvulsants, etc.), and low bone mass (osteopenia).[1] Certain medical conditions can also increase the risk of developing osteoporosis, either due to effects of the disease itself, the medications used to treat the condition, or both. This includes epilepsy, multiple sclerosis, Parkinson’s disease, stroke, COPD, adrenal insufficiency, Cushing’s syndrome, inflammatory bowel disease, multiple myeloma, sickle cell disease, HIV, and many others.[2]
Examine Database: Osteoporosis
Unlock the full potential of Examine
Research FeedRead all studies
In this meta-analysis of randomized controlled trials, Asian herbal medicine taken alongside calcium and/or vitamin D supplements was more effective than calcium and/or vitamin D supplements alone for increasing lumbar and femoral neck bone mineral density in participants with primary osteoporosis.
Frequently asked questions
Osteoporosis is a disease that thins and weakens the bones. Bones become fragile and fracture (break) easily, especially the bones in the hip, spine, and wrist. In the United States, millions of people either already have osteoporosis or are at high risk due to low bone mass. Osteoporosis is a silent disease, meaning some people don’t know they have it until a bone is broken.[1]
Osteoporosis is diagnosed by bone mineral density (BMD) of the spine or hip, which is measured with dual energy x-ray absorptiometry (DEXA) scans. A normal BMD is no more than 1 standard deviation (SD) below the average or reference value. Osteopenia (low bone mass) is 1-2.5 SDs below the reference and osteoporosis is 2.5 SD or more below the reference BMD value.[2]
The main goal of treating osteoporosis is to prevent fractures. This is done by strengthening the bones and by preventing falls. Medication treatments to strengthen the bones include bisphosphonates (alendronate, risedronate, etc.), raloxifene (Evista), calcitonin, and for more severe osteoporosis teriparatide (Forteo) and denosumab (Prolia).[2]
Many supplements have been studied for osteoporosis. Adequate calcium and vitamin D is important for preventing and treating osteoporosis, so if there’s not enough in the diet, a dietary supplement is recommended.[2] Other supplements such as multivitamins, vitamin K, and probiotics might also have some benefit, but higher quality research is needed.[3][4][5]
Low circulating vitamin D (25(OH)D) concentrations have been associated with bone health outcomes including an increased risk of falls and low bone mineral density in some populations, suggesting that low vitamin D levels are a risk factor for osteoporosis.[24]
A recent statement from the U.S. Preventive Services Task Force concluded that the current evidence is insufficient to conclude a benefit of vitamin D or calcium supplementation on fracture prevention in men and women who do not have a known vitamin D deficiency, osteoporosis, or prior fracture.[25][26] However, some studies have found that vitamin D — especially when combined with calcium supplementation — can increase bone mineral density and reduce the risk of fractures and falls in certain populations.[24]
Research is still scarce, but current evidence suggests that, through their effect on calcium regulation, some forms of vitamin K can help prevent osteoporosis and cardiovascular diseases.
Vitamin K is poorly understood, both by the general public and among health professionals. It has a wide range of potential benefits, but their nature and extent are still uncertain.
Why is that?
Some vitamins are more popular than others. In the past, a lot of research went into vitamin C, which became a popular supplement. Nowadays, a lot of research goes into vitamin D, whose popularity as a supplement is steadily growing.
By contrast, research on vitamin K is still scarce, having slowly developed over the past two decades. Further, it is scattered, because there exist several forms of vitamin K. Some of those forms are present only in a few foods. Others exist in various foods, but only in minute amounts. Few have been the subject of human trials.
The human trials that do exist, however, are overall promising. In order to understand their value and limitations, first you need to know a few basic facts. So let’s begin:
What is vitamin K?
Of the four fat-soluble vitamins (A, D, E, and K), vitamin K was discovered last. In 1929, Danish scientist Henrik Dam discovered a compound that played a role in coagulation (blood clotting).[47] When he first published his findings, in a German journal, he called this compound Koagulationsvitamin, which became known as vitamin K.
Today, we know that vitamin K participates in some very important biological processes, notably the carboxylation of calcium-binding proteins (including osteocalcin and matrix GLA protein).[48] In other words, vitamin K helps modify proteins so they can bind calcium ions (Ca2+). Through this mechanism, vitamin K partakes in blood clotting, as Henrik Dam discovered, but also of calcium regulation: it helps ensure that more calcium gets deposited in bones and less in soft tissues, thus strengthening bones and reducing arterial stiffness.
What complicates matters is that each vitamin has different forms, called vitamers, each of which may affect you differently. Vitamin K has natural vitamers, K1 (phylloquinone) and K2 (menaquinone), and synthetic vitamers, the best-known of which is K3 (menadione).
Vitamin K1
K1 is produced in plants, where it is involved in photosynthesis: the greener the plant, the greater its chlorophyll content; the greater its chlorophyll content, the greater its K1 content. When it comes to foods, K1 is especially abundant in green leafy vegetables.
K1 makes for 75–90% of the vitamin K in the Western diet.[49] Unfortunately, K1 is tightly bound to chloroplasts (organelles that contain chlorophyll and conduct photosynthesis), so you could be absorbing very little of what you eat[50] — maybe less than 10%.[51] Since vitamin K is a fat-soluble vitamin, however, its absorption can be enhanced by the co-ingestion of fat: adding fat to cooked spinach can raise K1 bioavailability from 5% to 13%.[52]
Vitamin K2
Things become more complicated here, because just as there are several forms of vitamin K, there are several forms of vitamin K2. To be more precise, the side chain of K1 always has four isoprenoid units (five-carbon structures), so there is only one form of K1, but the side chain of K2 has n isoprenoid units, so there are n forms of K2, called MK-n.[53][54]
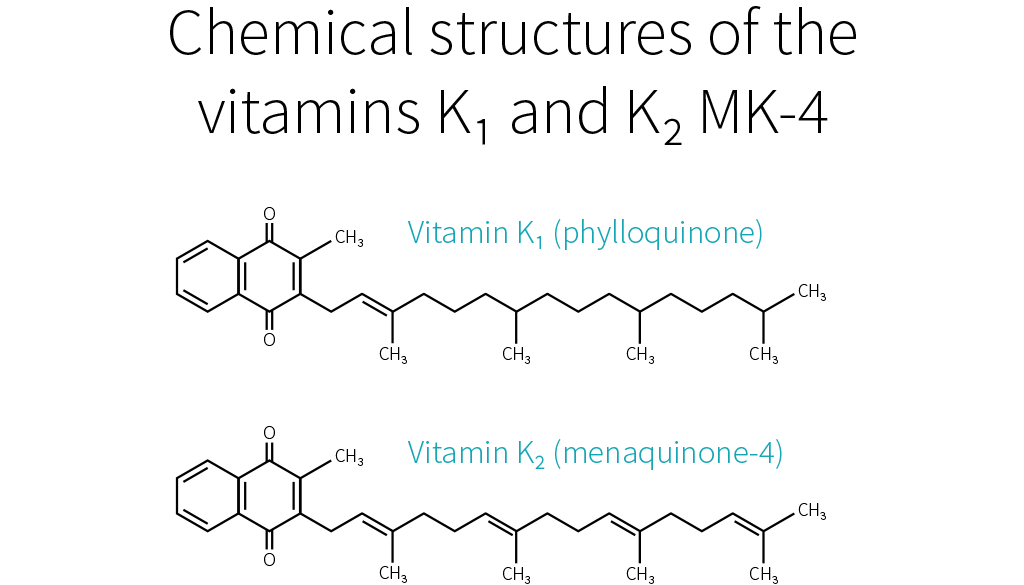
Whereas the side chain of K1 has four saturated isoprenoid units, the side chain of K2 MK-4 has four unsaturated isoprenoid units. Although K1 is directly active in your system, your body can also convert it to MK-4.[55][56][57] How much gets converted depends notably on your genetic heritage.[49]
MK-4 is present in animal products (meat, eggs, and dairy), though only in small quantities. Because those foods usually contain fat, dietary MK-4 should be better absorbed than dietary K1,[58] but future studies will need to confirm this hypothesis.

Other than MK-4, all forms of K2 are produced by bacteria. Your microbiota was once thought to produce three-fourths of the vitamin K you absorb.[59] Vitamin K, however, is mostly produced in the colon, where there are no bile salts to facilitate its absorption, so the actual ratio is probably much lower.[58][60]
Bacteria-produced K2 can be found in fermented foods, such as cheese and curds, but also in liver meat.[61] The richest dietary source of K2 is natto (fermented soybeans), which contains mostly MK-7.[62][63] As it stands, MK-7 is the only form of K2 that can be consumed in supplemental doses through food (i.e., natto). For that reason, MK-7 is the most-studied form of K2, together with MK-4.
K1 and MK-4 both have a side chain composed of four isoprenoid units; their half-life in your blood is 60–90 minutes. MK-7 has a side chain composed of seven isoprenoid units; it remains in your blood for several days. Due to their different side-chain lengths, the various forms tend to be transported on different lipoproteins, which are taken up at different rates by various tissues.[64][65][66][67][68] K1 and MK-4 are used quickly (K1 in the liver, MK-4 in other specific tissues), whereas MK-7 has more time to travel and be used throughout the body (which makes it, in theory, the best option for bone health).
Vitamin K3
K1 and K2 are the only natural forms of vitamin K, but there exist several synthetic forms, the best known of which is K3. However, whereas the natural forms of vitamin K are safe, even in high doses, K3 can interfere with glutathione, your body’s main antioxidant. K3 was once used to treat vitamin K deficiency in infants, but it caused liver toxicity, jaundice, and hemolytic anemia. Nowadays, it is used only in animal feed, in small doses. In the animals, vitamin K3 gets converted into K2 MK-4,[69] which you can consume safely.
Vitamin K is a family of fat-soluble vitamins. K1 and K2, the natural forms, are safe even in high doses. There is only one type of K1; it is found in plants, notably green leafy vegetables; your body can use it directly or convert it to K2 MK-4. Aside from MK-4, all other types of K2 are produced by bacteria, including the bacteria populating your gut. MK-4 is present in animal products (meat, eggs, dairy), whereas other types of K2 can be found in fermented foods and liver meat.
Vitamin K and your health
As far as we know, vitamin K mainly affects bloodclotting, cardiovascular health, and bone health. Epidemiological studies have mostly focused on K1; cardiovascular trials, on K1 and MK-7 (the main type present in natto, the richest dietary source of K2); bone trials, on MK-4 (the type of K2 your body can make out of K1).
Blood clotting
Vitamin K deficiency impairs blood clotting, causing excessive bleeding and bruising. It is rare in adults, but more common in newborns (more than 4 cases per 100,000 births in the UK[70]), where it can result in life-threatening bleeding within the skull. For that reason, the American Academy of Pediatrics recommends that newborns receive K1 shortly after birth (intramuscular injections have shown greater efficacy than oral administration).[71]
If you suffer from hypercoagulation (if your blood clots too easily), you might be prescribed a vitamin K antagonist (VKA), such as warfarin, a medication that hinders the recycling of vitamin K. Some doctors recommend that VKA users shun vitamin K entirely, but preliminary evidence suggests that, under professional supervision, vitamin K supplements might help stabilize the effects of VKAs.[61]
Which form should be supplemented, though, and in what amount, is still uncertain. There is some evidence that K1 enhances coagulation more than does MK-4[72][73] but less than does MK-7.[66] With regard to daily supplementation, 100 μg of K1 is considered safe, but in some people 10 μg of MK-7 is enough to significantly impair VKA therapy.[74]
Remember that natto is rich in MK-7. A single serving of natto can increase blood clotting for up to four days,[75] so it is one food VKA users should avoid. Other foods should be safe to eat. Please note that in people who do not suffer from hypercoagulation, and thus do not need to medicate with VKA, high intakes of natto have never been correlated to excessive blood clotting. Similarly, human studies saw no increase in blood-clot risk even from 45 mg (45,000 μg) of MK-4 taken once[76] or even thrice[77] daily.
Cardiovascular health
As we saw, vitamin K partakes in calcium regulation: it helps ensure that more calcium gets deposited in bones and less in soft tissues, thus reducing arterial stiffness. This is why people who take vitamin K antagonists, such as warfarin, are more likely to suffer from vascular calcification.[78][79]
Epidemiological studies[80][81][82] and mechanistic evidence[83] suggest that dietary K2 benefits cardiovascular health more than an equal dose of dietary K1.
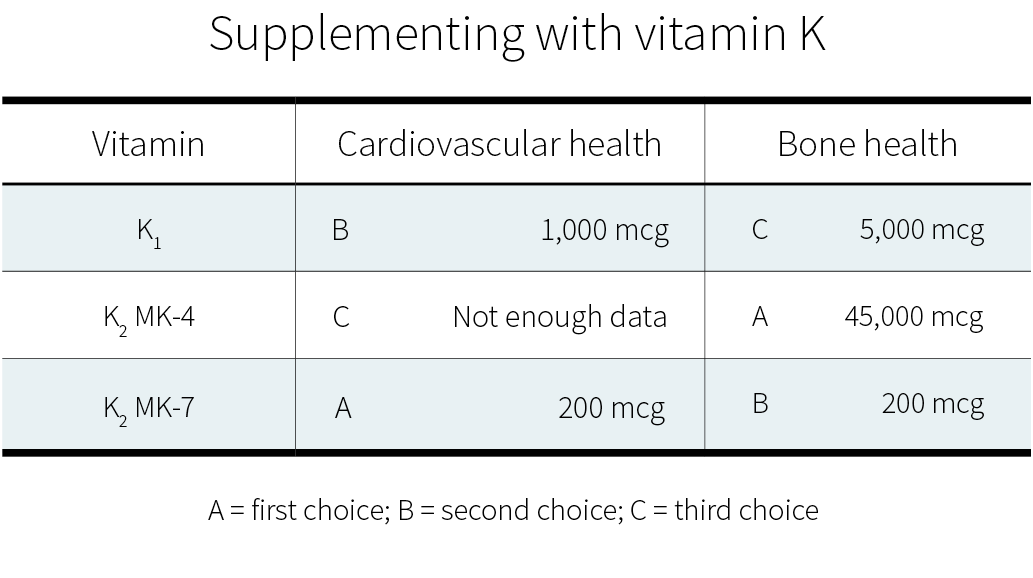
Clinical trials on supplemental vitamin K have focused on K1[84][85] and MK-7.[86][87][88] Often, those trials used a combination of vitamin D and other nutrients, but with vitamin K being the key difference between the intervention group and the control groups. Both of these forms of vitamin K seem to cause a consistent reduction in arterial stiffness (with better evidence for MK-7), and less consistent reductions in coronary calcification and carotid intima-media thickness. Judging from those trials and the epidemiological evidence, MK-7 seems the better choice.
Bone health
As we have just seen again, vitamin K partakes in calcium regulation: it helps ensure that less calcium gets deposited in soft tissues and more in bones, thus strengthening the latter. This is why people who take vitamin K antagonists, such as warfarin, might be more at risk of bone fractures,[89][90] though not all studies agree they are.[91]
Current evidence suggests that supplementing with vitamin K — or, at least, with certain forms of vitamin K — can benefit bone health, especially in the elderly (who have lower levels of circulating K2).[92] This potential should be explored, since, as the world population grows (and grows older), so does the number of osteoporotic fractures.[93] [94][95]
MK-7 appears to support the carboxylation of osteocalcin (a major calcium-binding protein in bones) more efficiently than K1.[66] Clinical trials suggest that, for the purpose of increasing bone density, MK-4 and MK-7 work more reliably than K1.[96]
More significantly, a meta-analysis of MK-4 trials found an overall decrease in fracture risk.[97] The effect of K1 or MK-7 supplementation on fracture risk is less clear. Only one K1 trial looked at fracture risk; it reported a decrease, but without a concomitant increase in bone mineral density.[98] Of the two MK-7 trials, one reported no difference in the number of fractures between the placebo group and the MK-7 group,[99] whereas the other reported fewer fractures in the MK-7 group;[100] there were, however, no statistical analyses for either study.
More research on vitamin K and fracture risk will be needed to clarify the effects of the different forms at different dosages. Currently, if you wish to supplement for bone health, a very high dose of MK-4 (45,000 μg) is the option best supported by human studies.[97] Those studies, all in Japanese people, focused on the prevention of bone fractures, and yes, much smaller dosages can probably help support bone health; but how much smaller?
In a 12-month study, 20 patients suffering from a chronic kidney disorder were given a daily glucocorticoid (a corticosteroid that has for side effect to decrease bone formation and increase bone resorption). In addition, half the patients received 15 mg of MK-4 daily, while the other half received a placebo. The placebo group experienced bone-density loss (BDL) in the lumbar spine, while the MK-4 group did not.[101]
More recently, a 12-month study in 48 postmenopausal Japanese women gave 1.5 mg of MK-4 daily to half of them and found a significant reduction in forearm BDL, but not in hip BDL, and it didn’t evaluate fractures.[102]
So there is some evidence for dosages lower than 45 mg/day. It is, however, a lot weaker.
In healthy people, vitamin K supplementation does not increase the risk of blood clots. Judging from limited evidence, MK-7 seems to be the best form of vitamin K for cardiovascular health, and MK-4 the best form of vitamin K for bone health.
How much vitamin K do you need?
Since vitamin K is crucial to your health, why is it the subject of relatively few studies? One of the reasons is simply that vitamin K deficiency is very rare in healthy, well-fed adults. It is mostly a concern in newborns, in people who have been prescribed a vitamin K antagonist, in people who suffer from severe liver damage, and in people who have problems absorbing fat.[103][104][105]
Vitamin K is abundant in a balanced diet, and the bacteria in your colon can also produce some. Moreover, your body can recycle it many times, and this vitamin K-epoxide cycle more than makes up for the limited ability your body shows for storing vitamin K.
Still, you can recycle vitamin K many times, but not forever, and so you still need to consume some regularly. But how much, exactly?
No one knows. There is, as yet, not enough evidence to set a Recommended Dietary Allowance (RDA) for vitamin K, so an Adequate Intake (AI) has been established at a level assumed to prevent excessive bleeding. In the United States, the AI for vitamin K is 120 μg/day for men and 90 μg/day for women. In Europe, the AI for vitamin K is 70 μg/day for men and women. More recent research, however, suggests that those numbers should be increased.[65]
Since 100 g of collards contain, on average, 360 μg of vitamin K,[106][53] getting enough vitamin K looks easy. But can’t you just as easily get too much?
Fortunately, no. Though allergic reactions have occurred with vitamin K injections,[107][108][109] no incidence of actual toxicity has ever been reported in people taking natural vitamin K, even in high supplemental doses.[110] For that reason, neither the FDA nor the EFSA has set a Tolerable Upper Intake Level (UL) for vitamin K. One should note, however, that we lack long-term, high-dose studies on vitamin K safety.
Sources of vitamin K
K1 can be found in plant products, notably green leafy vegetables. K2 MK-4 can be found in animal products (meat, eggs, and dairy). The other types of K2 can be found in fermented foods and liver meat.

Table references: [111][112][53][113][114][68][106][115][116]
Meats’ vitamin K content correlates positively but non-linearly with their fat content and will vary according to the animal’s diet (and thus country of origin). Forms of K2 other than MK-4 and MK-7 have not been well studied but are likely to have some benefit — cheeses and beef liver are notable sources of others forms of K2[112][116] and cheese consumption is associated with a reduced risk of cardiovascular disease.[117]
While well-conducted controlled trials provide the most reliable evidence, most such trials used amounts of vitamin K2 that far exceed what could be obtained through foods, save for natto. This leaves us wondering if dietary K2 has any effect.
Fortunately, it seems to be the case: a high dietary intake of K2 (≥33 μg/day seems optimal) may reduce the risk of coronary heart disease — an effect a high dietary intake of K1 doesn’t appear to have.[80][82][81][118] It doesn’t mean, of course, that foods rich in K1 are valueless: dietary K1 intake will protect you from excessive bleeding and is inversely associated with risk of bone fractures.[119]
Observational studies, however, are less reliable than controlled trials, so we know less about the effects of dietary intake than about the effects of supplemental intake. If you wish to supplement with vitamin K, here are the dosages supported by the current evidence:
Summary
Although much more research needs to be performed, there is early evidence that vitamin K, whether in food or in supplemental form, can benefit cardiovascular health and bone health.

To keep bones strong and to prevent osteoporosis, a healthy diet sufficient in calcium and vitamin D is recommended.[2] A meta-analysis of observational research has found that Western diets involving fast food, refined foods, meats and sugar are associated with lower BMD in contrast to a Mediterranean diet pattern or dietary pattern higher in dairy.[6][7]
More protein in the diet has been linked to more calcium in the urine. Two reasons have been suggested to explain this phenomenon:
- Your body draws from its calcium stores (in bones) to buffer the acid load caused by dietary protein. This has led researchers to suggest that higher protein intake could increase bone loss.[13]
- Most studies that looked at protein intake and calcium excretion list dairy products as a protein source,[14] so higher urinary calcium could simply be the result of higher calcium intake (i.e., more calcium in, more calcium out).
Therefore, looking only at calcium excretion wasn’t enough. Subsequent studies showed that dietary protein promotes dietary-calcium absorption[15] and that high protein intake “promotes bone growth and retards bone loss whereas low-protein diet is associated with higher risk of hip fractures.”[16] High-protein diets have also been shown to modestly suppress the decrease in bone mineral density caused by weight loss.[17]
What happens is that when you ingest more protein, you absorb more of the calcium in your food, so less calcium ends up in your feces. Later, your body gets rid of the calcium it doesn’t need, so more calcium ends up in your urine, but not as much as would have otherwise ended in your feces.[18] Therefore, an increase in protein intake leads to an overall decrease in calcium excretion, which points to an increase in calcium retention. High-protein diets also raise your insulin-like growth factor-1 (IGF-1),[19] which notably promotes bone growth.[20]
All in all, current evidence suggests that protein’s effect on bones is either neutral or beneficial.[18][21]
One of the key goals of treating osteoporosis is to prevent fractures by preventing falls. Exercise that involves strength and balance training helps to prevent falls. Other recommendations which may reduce the risk of fractures include limiting alcohol and caffeine intake, stopping smoking, and increasing exposure to sunlight.[2]
Mechanical loading of bone through weight-bearing exercise is one of the best ways to increase bone mineral density and therefore, exercise has been suggested to prevent and treat osteoporosis — but the type of exercise matters. Running, weight training, and high-impact aerobic exercise can increase bone mineral density in the hips and spine. Gentle, low-impact aerobic exercise and walking protect against further losses in bone mineral density, while swimming does not seem to have a beneficial effect.[27] It appears that adolescents and prepubertal girls derive the greatest benefit from weight-bearing exercise when it comes to increasing their peak bone mass. Jumping, hopping, weight training, and high-impact exercise are the most effective forms of activity for increasing bone mineral density in most populations. In terms of duration, 2-4 exercise sessions per week lasting 30 minutes or less can be effective for maintaining and improving bone quality.[28]
Resistance training can increase muscle mass, protect bone mineral density, and reduce the risk of diabetes.
Lifting weights, or resistance training, has numerous benefits to the muscles and skeleton that are uniquely attributed to this form of training.
There are some cognitive benefits associated with exercise in general, but this FAQ entry will be more focused on what resistance training can give that other forms of exercise cannot.
Resistance training?
Resistance training is a form of training where the muscles and skeleton are pit against a large force, either induced by external resistance (lifting weights) or by gravity (maximal jumping or sprinting). Resistance training tends to be focused on power, and tends to be anaerobic (intense) in nature.
Anything with maximal exertions can be considered resistance training. Things like Tennis and racquetball show some benefits as well due to some strides being full exertion, but weightlifting tends to have the most dramatic effects.
Benefits to Muscles
Most notably weight lifting, but all forms of resistance training, can increase muscle mass.
This can reduce the occurrence of sarcopenia (the age-related decline in muscle mass not associated with pro-inflammatory cytokines)[29] when elderly,[30][31] although all activity can reduce rates of sarcopenia, resistance training seems most effective.[32][33]
Benefits to Bone
Exercise in general tends to be associated with better bone mineral density and/or bone width in athletes when compared to a non-athletic control group.[34][35][36] Greater bone health and an exercise regimen are inversely associated with falls in the elderly, which suggests that exercise is a good preventative measure.[37][38][39]
It might also slightly protect against further reductions in bone mineral density in those already diagnosed with osteoporosis or osteopenia,[40] although in general activity is encouraged.[41]
In older age, those who practice Sprinting have been shown to have better bone density and size relative to jogging and walking activities.[42] Although beneficial bone adaptations seem to be better in the young, they can still occur even if one starts a physical exercise program later in life.[43]
It should be noted that swimming does not tend to increase bone density or mass, as the person is suspended in a pool of water rather than actively forcing power against gravity. It may increase bone health slighty in some persons, but is much less reliable than other forms of exercise.[41][44][45]
Health Promoting effects
Involvement in exercise for at least 150 minutes a week in associated with a reduced risk of diabetes in men, with a protective effect existing for both aerobic exercise and weight training with persons participating in both having least risk.[46]
Anyone can develop osteoporosis, but it is more common in females of older age. Risk factors for getting osteoporosis include old age, low body weight, family history, smoking, certain medications (corticosteroids, anticonvulsants, etc.), and low bone mass (osteopenia).[1] Certain medical conditions can also increase the risk of developing osteoporosis, either due to effects of the disease itself, the medications used to treat the condition, or both. This includes epilepsy, multiple sclerosis, Parkinson’s disease, stroke, COPD, adrenal insufficiency, Cushing’s syndrome, inflammatory bowel disease, multiple myeloma, sickle cell disease, HIV, and many others.[2]
Bone mass is, for the most part, regulated by the activity of two specialized cell types. Osteoblasts are tasked with adding bone mass, while osteoclasts actively digest it and cause bone resorption. In the context of diseases like osteoporosis, increasing osteoclast number or activity shifts the balance toward bone resorption, causing a progressive loss of bone density over time.[8] Bone is capable of sensing mechanical stress, which lessens in response to weight loss. This shifts the balance of bone remodeling cells. Calorie restriction also alters a number of hormones that play a role in the regulation of bone mass. Reductions in body fat have been linked to reduced levels of estrogen and other sex hormones,[9] and increased sex hormone binding globulin (SHBG), a protein that binds to and sequesters hormones, blocking their function. Although shifts in overall hormone levels during calorie restriction and weight loss can be subtle, small changes in hormone levels (particularly estrogens, and IGF-1)[10][11][12] can work through both direct and indirect mechanisms to alter the balance of osteoblast vs. osteoclasts activity to promote bone resorption and decreased bone density.
It is a common misconception that osteoporosis is a “woman’s disease.” Although women do tend to experience osteoporosis more than men and experience the condition at a younger age, men can also get osteoporosis. Osteoporosis tends to begin at a later age in men — around 70 years of age or so compared to 50 years in women.[22] Risk factors for male osteoporosis include low testosterone levels, vitamin D deficiency, poor calcium intake, tobacco and heavy alcohol use, and prolonged use of some medications, including glucocorticoids (a type of steroid).[23]
References
- ^MedlinePlus (Internet) Bethesda (MD): National Library of Medicine (US); (updated 2022 January 26)
- ^Jeremiah MP, Unwin BK, Greenawald MH, Casiano VEDiagnosis and Management of Osteoporosis.Am Fam Physician.(2015-Aug-15)
- ^Beeram I, Mortensen SJ, Yeritsyan D, Momenzadeh K, von Keudell A, Nazarian AMultivitamins and risk of fragility hip fracture: a systematic review and meta-analysis.Arch Osteoporos.(2021-02-11)
- ^Mott A, Bradley T, Wright K, Cockayne ES, Shearer MJ, Adamson J, Lanham-New SA, Torgerson DJEffect of vitamin K on bone mineral density and fractures in adults: an updated systematic review and meta-analysis of randomised controlled trials.Osteoporos Int.(2019-Aug)
- ^Emma O Billington, Amita Mahajan, Jamie L Benham, Maitreyi RamanEffects of probiotics on bone mineral density and bone turnover: A systematic reviewCrit Rev Food Sci Nutr.(2021 Nov 8)
- ^Fabiani R, Naldini G, Chiavarini MDietary Patterns in Relation to Low Bone Mineral Density and Fracture Risk: A Systematic Review and Meta-Analysis.Adv Nutr.(2019-03-01)
- ^Malmir H, Saneei P, Larijani B, Esmaillzadeh AAdherence to Mediterranean diet in relation to bone mineral density and risk of fracture: a systematic review and meta-analysis of observational studies.Eur J Nutr.(2018-Sep)
- ^Tu KN, Lie JD, Wan CKV, Cameron M, Austel AG, Nguyen JK, Van K, Hyun DOsteoporosis: A Review of Treatment OptionsP T.(2018 Feb)
- ^O'Dea JP, Wieland RG, Hallberg MC, Llerena LA, Zorn EM, Genuth SMEffect of dietery weight loss on sex steroid binding sex steroids, and gonadotropins in obese postmenopausal womenJ Lab Clin Med.(1979 Jun)
- ^Eriksen EF, Colvard DS, Berg NJ, Graham ML, Mann KG, Spelsberg TC, Riggs BLEvidence of estrogen receptors in normal human osteoblast-like cellsScience.(1988 Jul 1)
- ^Heino TJ, Hentunen TA, Väänänen HKOsteocytes inhibit osteoclastic bone resorption through transforming growth factor-beta: enhancement by estrogenJ Cell Biochem.(2002)
- ^Oster MH, Fielder PJ, Levin N, Cronin MJAdaptation of the growth hormone and insulin-like growth factor-I axis to chronic and severe calorie or protein malnutritionJ Clin Invest.(1995 May)
- ^Barzel US, Massey LKExcess dietary protein can adversely affect boneJ Nutr.(1998 Jun)
- ^Schwingshackl L, Hoffmann GComparison of high vs. normal/low protein diets on renal function in subjects without chronic kidney disease: a systematic review and meta-analysisPLoS One.(2014 May 22)
- ^Hunt JR, Johnson LK, Fariba Roughead ZKDietary protein and calcium interact to influence calcium retention: a controlled feeding studyAm J Clin Nutr.(2009 May)
- ^Shams-White MM, Chung M, Du M, Fu Z, Insogna KL, Karlsen MC, LeBoff MS, Shapses SA, Sackey J, Wallace TC, Weaver CMDietary protein and bone health: a systematic review and meta-analysis from the National Osteoporosis FoundationAm J Clin Nutr.(2017 Jun)
- ^Wright CS, Li J, Campbell WWEffects of Dietary Protein Quantity on Bone Quantity following Weight Loss: A Systematic Review and Meta-analysisAdv Nutr.(2019 Nov 1)
- ^Calvez J, Poupin N, Chesneau C, Lassale C, Tomé DProtein intake, calcium balance and health consequencesEur J Clin Nutr.(2012 Mar)
- ^Livingstone CInsulin-like growth factor-I (IGF-I) and clinical nutritionClin Sci (Lond).(2013 Sep)
- ^Yakar S, Rosen CJ, Beamer WG, Ackert-Bicknell CL, Wu Y, Liu JL, Ooi GT, Setser J, Frystyk J, Boisclair YR, LeRoith DCirculating levels of IGF-1 directly regulate bone growth and densityJ Clin Invest.(2002 Sep)
- ^Fenton TR, Lyon AW, Eliasziw M, Tough SC, Hanley DAMeta-analysis of the effect of the acid-ash hypothesis of osteoporosis on calcium balanceJ Bone Miner Res.(2009 Nov)
- ^Heather Buschman PhDBreaking Dad: Osteoporosis and Its Consequences Affect Men Too
- ^Herrera A, Lobo-Escolar A, Mateo J, Gil J, Ibarz E, Gracia LMale osteoporosis: A review.World J Orthop.(2012-Dec-18)
- ^Cranney A, Horsley T, O'Donnell S, Weiler H, Puil L, Ooi D, Atkinson S, Ward L, Moher D, Hanley D, Fang M, Yazdi F, Garritty C, Sampson M, Barrowman N, Tsertsvadze A, Mamaladze VEffectiveness and safety of vitamin D in relation to bone health.Evid Rep Technol Assess (Full Rep).(2007-Aug)
- ^Moyer VA,Vitamin D and calcium supplementation to prevent fractures in adults: U.S. Preventive Services Task Force recommendation statement.Ann Intern Med.(2013-May-07)
- ^Kahwati LC, Weber RP, Pan H, Gourlay M, LeBlanc E, Coker-Schwimmer M, Viswanathan MVitamin D, Calcium, or Combined Supplementation for the Primary Prevention of Fractures in Community-Dwelling Adults: Evidence Report and Systematic Review for the US Preventive Services Task Force.JAMA.(2018-04-17)
- ^Todd JA, Robinson RJOsteoporosis and exercise.Postgrad Med J.(2003-Jun)
- ^Troy KL, Mancuso ME, Butler TA, Johnson JEExercise Early and Often: Effects of Physical Activity and Exercise on Women's Bone Health.Int J Environ Res Public Health.(2018-04-28)
- ^Thomas DRSarcopeniaClin Geriatr Med.(2010 May)
- ^Sundell JResistance Training Is an Effective Tool against Metabolic and Frailty SyndromesAdv Prev Med.(2011)
- ^Johnston AP, De Lisio M, Parise GResistance training, sarcopenia, and the mitochondrial theory of agingAppl Physiol Nutr Metab.(2008 Feb)
- ^Pillard F, Laoudj-Chenivesse D, Carnac G, Mercier J, Rami J, Rivière D, Rolland YPhysical activity and sarcopeniaClin Geriatr Med.(2011 Aug)
- ^Bautmans I, Van Puyvelde K, Mets TSarcopenia and functional decline: pathophysiology, prevention and therapyActa Clin Belg.(2009 Jul-Aug)
- ^Kemmler W, von Stengel S, Engelke K, Häberle L, Kalender WAExercise effects on bone mineral density, falls, coronary risk factors, and health care costs in older women: the randomized controlled senior fitness and prevention (SEFIP) studyArch Intern Med.(2010 Jan 25)
- ^Taaffe DR, Robinson TL, Snow CM, Marcus RHigh-impact exercise promotes bone gain in well-trained female athletesJ Bone Miner Res.(1997 Feb)
- ^Martyn-St James M, Carroll SEffects of different impact exercise modalities on bone mineral density in premenopausal women: a meta-analysisJ Bone Miner Metab.(2010 May)
- ^Hourigan SR, Nitz JC, Brauer SG, O'Neill S, Wong J, Richardson CAPositive effects of exercise on falls and fracture risk in osteopenic womenOsteoporos Int.(2008 Jul)
- ^Kronhed AC, Möller MEffects of physical exercise on bone mass, balance skill and aerobic capacity in women and men with low bone mineral density, after one year of training--a prospective studyScand J Med Sci Sports.(1998 Oct)
- ^Asikainen TM, Kukkonen-Harjula K, Miilunpalo SExercise for health for early postmenopausal women: a systematic review of randomised controlled trialsSports Med.(2004)
- ^de Matos O, Lopes da Silva DJ, Martinez de Oliveira J, Castelo-Branco CEffect of specific exercise training on bone mineral density in women with postmenopausal osteopenia or osteoporosisGynecol Endocrinol.(2009 Sep)
- ^Yamazaki S, Ichimura S, Iwamoto J, Takeda T, Toyama YEffect of walking exercise on bone metabolism in postmenopausal women with osteopenia/osteoporosisJ Bone Miner Metab.(2004)
- ^Wilks DC, Winwood K, Gilliver SF, Kwiet A, Chatfield M, Michaelis I, Sun LW, Ferretti JL, Sargeant AJ, Felsenberg D, Rittweger JBone mass and geometry of the tibia and the radius of master sprinters, middle and long distance runners, race-walkers and sedentary control participants: a pQCT studyBone.(2009 Jul)
- ^Kontulainen S, Sievänen H, Kannus P, Pasanen M, Vuori IEffect of long-term impact-loading on mass, size, and estimated strength of humerus and radius of female racquet-sports players: a peripheral quantitative computed tomography study between young and old starters and controlsJ Bone Miner Res.(2003 Feb)
- ^Derman O, Cinemre A, Kanbur N, Doğan M, Kiliç M, Karaduman EEffect of swimming on bone metabolism in adolescentsTurk J Pediatr.(2008 Mar-Apr)
- ^Taaffe DR, Snow-Harter C, Connolly DA, Robinson TL, Brown MD, Marcus RDifferential effects of swimming versus weight-bearing activity on bone mineral status of eumenorrheic athletesJ Bone Miner Res.(1995 Apr)
- ^A Prospective Study of Weight Training and Risk of Type 2 Diabetes Mellitus in Men
- ^Dam HThe antihaemorrhagic vitamin of the chickBiochem J.(1935 Jun)
- ^Booth SLRoles for vitamin K beyond coagulationAnnu Rev Nutr.(2009)
- ^Shearer MJ, Newman PRecent trends in the metabolism and cell biology of vitamin K with special reference to vitamin K cycling and MK-4 biosynthesisJ Lipid Res.(2014 Mar)
- ^Garber AK, Binkley NC, Krueger DC, Suttie JWComparison of phylloquinone bioavailability from food sources or a supplement in human subjectsJ Nutr.(1999 Jun)
- ^Gijsbers BL, Jie KS, Vermeer CEffect of food composition on vitamin K absorption in human volunteersBr J Nutr.(1996 Aug)
- ^Ageno W, Gallus AS, Wittkowsky A, Crowther M, Hylek EM, Palareti GOral anticoagulant therapy: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice GuidelinesChest.(2012 Feb)
- ^Booth SLVitamin K: food composition and dietary intakesFood Nutr Res.(2012)
- ^Kurosu M, Begari EVitamin K2 in electron transport system: are enzymes involved in vitamin K2 biosynthesis promising drug targets?Molecules.(2010 Mar 10)
- ^Shearer MJ, Newman PMetabolism and cell biology of vitamin KThromb Haemost.(2008 Oct)
- ^Davidson RT, Foley AL, Engelke JA, Suttie JWConversion of dietary phylloquinone to tissue menaquinone-4 in rats is not dependent on gut bacteriaJ Nutr.(1998 Feb)
- ^Ronden JE, Drittij-Reijnders MJ, Vermeer C, Thijssen HHIntestinal flora is not an intermediate in the phylloquinone-menaquinone-4 conversion in the ratBiochim Biophys Acta.(1998 Jan 8)
- ^Beulens JW, Booth SL, van den Heuvel EG, Stoecklin E, Baka A, Vermeer CThe role of menaquinones (vitamin K₂) in human healthBr J Nutr.(2013 Oct)
- ^Miggiano GA, Robilotta LVitamin K-controlled diet: problems and prospectsClin Ter.(2005 Jan-Apr)
- ^Ichihashi T, Takagishi Y, Uchida K, Yamada HColonic absorption of menaquinone-4 and menaquinone-9 in ratsJ Nutr.(1992 Mar)
- ^Holmes MV, Hunt BJ, Shearer MJThe role of dietary vitamin K in the management of oral vitamin K antagonistsBlood Rev.(2012 Jan)
- ^Ikeda Y, Iki M, Morita A, Kajita E, Kagamimori S, Kagawa Y, Yoneshima HIntake of fermented soybeans, natto, is associated with reduced bone loss in postmenopausal women: Japanese Population-Based Osteoporosis (JPOS) StudyJ Nutr.(2006 May)
- ^Katsuyama H, Ideguchi S, Fukunaga M, Saijoh K, Sunami SUsual dietary intake of fermented soybeans (Natto) is associated with bone mineral density in premenopausal womenJ Nutr Sci Vitaminol (Tokyo).(2002 Jun)
- ^Sato T, Schurgers LJ, Uenishi KComparison of menaquinone-4 and menaquinone-7 bioavailability in healthy womenNutr J.(2012 Nov 12)
- ^Vermeer CVitamin K: the effect on health beyond coagulation - an overviewFood Nutr Res.(2012)
- ^Schurgers LJ, Teunissen KJ, Hamulyák K, Knapen MH, Vik H, Vermeer CVitamin K-containing dietary supplements: comparison of synthetic vitamin K1 and natto-derived menaquinone-7Blood.(2007 Apr 15)
- ^Schurgers LJ, Vermeer CDifferential lipoprotein transport pathways of K-vitamins in healthy subjectsBiochim Biophys Acta.(2002 Feb 15)
- ^Schurgers LJ, Vermeer CDetermination of phylloquinone and menaquinones in food. Effect of food matrix on circulating vitamin K concentrationsHaemostasis.(2000 Nov-Dec)
- ^Nakagawa K, Hirota Y, Sawada N, Yuge N, Watanabe M, Uchino Y, Okuda N, Shimomura Y, Suhara Y, Okano TIdentification of UBIAD1 as a novel human menaquinone-4 biosynthetic enzymeNature.(2010 Nov 4)
- ^Shearer MJVitamin KLancet.(1995 Jan 28)
- ^American Academy of Pediatrics Committee on Fetus and NewbornControversies concerning vitamin K and the newborn. American Academy of Pediatrics Committee on Fetus and NewbornPediatrics.(2003 Jul)
- ^Spronk HM, Soute BA, Schurgers LJ, Thijssen HH, De Mey JG, Vermeer CTissue-specific utilization of menaquinone-4 results in the prevention of arterial calcification in warfarin-treated ratsJ Vasc Res.(2003 Nov-Dec)
- ^Groenen-van Dooren MM, Soute BA, Jie KS, Thijssen HH, Vermeer CThe relative effects of phylloquinone and menaquinone-4 on the blood coagulation factor synthesis in vitamin K-deficient ratsBiochem Pharmacol.(1993 Aug 3)
- ^Theuwissen E, Teunissen KJ, Spronk HM, Hamulyák K, Ten Cate H, Shearer MJ, Vermeer C, Schurgers LJEffect of low-dose supplements of menaquinone-7 (vitamin K2 ) on the stability of oral anticoagulant treatment: dose-response relationship in healthy volunteersJ Thromb Haemost.(2013 Jun)
- ^Schurgers LJ, Shearer MJ, Hamulyák K, Stöcklin E, Vermeer CEffect of vitamin K intake on the stability of oral anticoagulant treatment: dose-response relationships in healthy subjectsBlood.(2004 Nov 1)
- ^Ushiroyama T, Ikeda A, Ueki MEffect of continuous combined therapy with vitamin K(2) and vitamin D(3) on bone mineral density and coagulofibrinolysis function in postmenopausal womenMaturitas.(2002 Mar 25)
- ^Asakura H, Myou S, Ontachi Y, Mizutani T, Kato M, Saito M, Morishita E, Yamazaki M, Nakao SVitamin K administration to elderly patients with osteoporosis induces no hemostatic activation, even in those with suspected vitamin K deficiencyOsteoporos Int.(2001 Dec)
- ^Mayer O Jr, Seidlerová J, Bruthans J, Filipovský J, Timoracká K, Vaněk J, Cerná L, Wohlfahrt P, Cífková R, Theuwissen E, Vermeer CDesphospho-uncarboxylated matrix Gla-protein is associated with mortality risk in patients with chronic stable vascular diseaseAtherosclerosis.(2014 Jul)
- ^Chatrou ML, Winckers K, Hackeng TM, Reutelingsperger CP, Schurgers LJVascular calcification: the price to pay for anticoagulation therapy with vitamin K-antagonistsBlood Rev.(2012 Jul)
- ^Gast GC, de Roos NM, Sluijs I, Bots ML, Beulens JW, Geleijnse JM, Witteman JC, Grobbee DE, Peeters PH, van der Schouw YTA high menaquinone intake reduces the incidence of coronary heart diseaseNutr Metab Cardiovasc Dis.(2009 Sep)
- ^Beulens JW, Bots ML, Atsma F, Bartelink ML, Prokop M, Geleijnse JM, Witteman JC, Grobbee DE, van der Schouw YTHigh dietary menaquinone intake is associated with reduced coronary calcificationAtherosclerosis.(2009 Apr)
- ^Geleijnse JM, Vermeer C, Grobbee DE, Schurgers LJ, Knapen MH, van der Meer IM, Hofman A, Witteman JCDietary intake of menaquinone is associated with a reduced risk of coronary heart disease: the Rotterdam StudyJ Nutr.(2004 Nov)
- ^El Asmar MS, Naoum JJ, Arbid EJVitamin k dependent proteins and the role of vitamin k2 in the modulation of vascular calcification: a reviewOman Med J.(2014 May)
- ^Shea MK, O'Donnell CJ, Hoffmann U, Dallal GE, Dawson-Hughes B, Ordovas JM, Price PA, Williamson MK, Booth SLVitamin K supplementation and progression of coronary artery calcium in older men and womenAm J Clin Nutr.(2009 Jun)
- ^Braam LA, Hoeks AP, Brouns F, Hamulyák K, Gerichhausen MJ, Vermeer CBeneficial effects of vitamins D and K on the elastic properties of the vessel wall in postmenopausal women: a follow-up studyThromb Haemost.(2004 Feb)
- ^Kurnatowska I, Grzelak P, Masajtis-Zagajewska A, Kaczmarska M, Stefańczyk L, Vermeer C, Maresz K, Nowicki MEffect of vitamin K2 on progression of atherosclerosis and vascular calcification in nondialyzed patients with chronic kidney disease stages 3-5Pol Arch Med Wewn.(2015)
- ^Knapen MH, Braam LA, Drummen NE, Bekers O, Hoeks AP, Vermeer CMenaquinone-7 supplementation improves arterial stiffness in healthy postmenopausal women. A double-blind randomised clinical trialThromb Haemost.(2015 May)
- ^Fulton RL, McMurdo ME, Hill A, Abboud RJ, Arnold GP, Struthers AD, Khan F, Vermeer C, Knapen MH, Drummen NE, Witham MDEffect of Vitamin K on Vascular Health and Physical Function in Older People with Vascular Disease--A Randomised Controlled TrialJ Nutr Health Aging.(2016 Mar)
- ^Caraballo PJ, Heit JA, Atkinson EJ, Silverstein MD, O'Fallon WM, Castro MR, Melton LJ 3rdLong-term use of oral anticoagulants and the risk of fractureArch Intern Med.(1999 Aug 9-23)
- ^Gage BF, Birman-Deych E, Radford MJ, Nilasena DS, Binder EFRisk of osteoporotic fracture in elderly patients taking warfarin: results from the National Registry of Atrial Fibrillation 2Arch Intern Med.(2006 Jan 23)
- ^Jamal SA, Browner WS, Bauer DC, Cummings SRWarfarin use and risk for osteoporosis in elderly women. Study of Osteoporotic Fractures Research GroupAnn Intern Med.(1998 May 15)
- ^Hodges SJ, Pilkington MJ, Shearer MJ, Bitensky L, Chayen JAge-related changes in the circulating levels of congeners of vitamin K2, menaquinone-7 and menaquinone-8Clin Sci (Lond).(1990 Jan)
- ^Pisani P, Renna MD, Conversano F, Casciaro E, Di Paola M, Quarta E, Muratore M, Casciaro SMajor osteoporotic fragility fractures: Risk factor updates and societal impactWorld J Orthop.(2016 Mar 18)
- ^Dhanwal DK, Dennison EM, Harvey NC, Cooper CEpidemiology of hip fracture: Worldwide geographic variationIndian J Orthop.(2011 Jan)
- ^Johnell O, Kanis JAAn estimate of the worldwide prevalence and disability associated with osteoporotic fracturesOsteoporos Int.(2006 Dec)
- ^Fang Y, Hu C, Tao X, Wan Y, Tao FEffect of vitamin K on bone mineral density: a meta-analysis of randomized controlled trialsJ Bone Miner Metab.(2012 Jan)
- ^Cockayne S, Adamson J, Lanham-New S, Shearer MJ, Gilbody S, Torgerson DJVitamin K and the prevention of fractures: systematic review and meta-analysis of randomized controlled trialsArch Intern Med.(2006 Jun 26)
- ^Cheung AM, Tile L, Lee Y, Tomlinson G, Hawker G, Scher J, Hu H, Vieth R, Thompson L, Jamal S, Josse RVitamin K supplementation in postmenopausal women with osteopenia (ECKO trial): a randomized controlled trialPLoS Med.(2008 Oct 14)
- ^Emaus N, Gjesdal CG, Almås B, Christensen M, Grimsgaard AS, Berntsen GK, Salomonsen L, Fønnebø VVitamin K2 supplementation does not influence bone loss in early menopausal women: a randomised double-blind placebo-controlled trialOsteoporos Int.(2010 Oct)
- ^Knapen MH, Drummen NE, Smit E, Vermeer C, Theuwissen EThree-year low-dose menaquinone-7 supplementation helps decrease bone loss in healthy postmenopausal womenOsteoporos Int.(2013 Sep)
- ^Sasaki N, Kusano E, Takahashi H, Ando Y, Yano K, Tsuda E, Asano YVitamin K2 inhibits glucocorticoid-induced bone loss partly by preventing the reduction of osteoprotegerin (OPG)J Bone Miner Metab.(2005)
- ^Koitaya N, Sekiguchi M, Tousen Y, Nishide Y, Morita A, Yamauchi J, Gando Y, Miyachi M, Aoki M, Komatsu M, Watanabe F, Morishita K, Ishimi YLow-dose vitamin K2 (MK-4) supplementation for 12 months improves bone metabolism and prevents forearm bone loss in postmenopausal Japanese womenJ Bone Miner Metab.(2013 May 24)
- ^Nowak JK, Grzybowska-Chlebowczyk U, Landowski P, Szaflarska-Poplawska A, Klincewicz B, Adamczak D, Banasiewicz T, Plawski A, Walkowiak JPrevalence and correlates of vitamin K deficiency in children with inflammatory bowel diseaseSci Rep.(2014 Apr 24)
- ^Jagannath VA, Fedorowicz Z, Thaker V, Chang ABVitamin K supplementation for cystic fibrosisCochrane Database Syst Rev.(2013 Apr 30)
- ^Nakajima S, Iijima H, Egawa S, Shinzaki S, Kondo J, Inoue T, Hayashi Y, Ying J, Mukai A, Akasaka T, Nishida T, Kanto T, Tsujii M, Hayashi NAssociation of vitamin K deficiency with bone metabolism and clinical disease activity in inflammatory bowel diseaseNutrition.(2011 Oct)
- ^Booth SL, Pennington JA, Sadowski JAFood sources and dietary intakes of vitamin K-1 (phylloquinone) in the American diet: data from the FDA Total Diet StudyJ Am Diet Assoc.(1996 Feb)
- ^Shiratori T, Sato A, Fukuzawa M, Kondo N, Tanno SSevere Dextran-Induced Anaphylactic Shock during Induction of Hypertension-Hypervolemia-Hemodilution Therapy following Subarachnoid HemorrhageCase Rep Crit Care.(2015)
- ^Riegert-Johnson DL, Volcheck GWThe incidence of anaphylaxis following intravenous phytonadione (vitamin K1): a 5-year retrospective reviewAnn Allergy Asthma Immunol.(2002 Oct)
- ^Bullen AW, Miller JP, Cunliffe WJ, Losowsky MSSkin reactions caused by vitamin K in patients with liver diseaseBr J Dermatol.(1978 May)
- ^Institute of Medicine (US) Panel on MicronutrientsDietary Reference Intakes for Vitamin A, Vitamin K, Arsenic, Boron, Chromium, Copper, Iodine, Iron, Manganese, Molybdenum, Nickel, Silicon, Vanadium, and Zinc
- ^Fu X, Shen X, Finnan EG, Haytowitz DB, Booth SLMeasurement of Multiple Vitamin K Forms in Processed and Fresh-Cut Pork Products in the U.S. Food SupplyJ Agric Food Chem.(2016 Jun 8)
- ^Manoury E, Jourdon K, Boyaval P, Fourcassié PQuantitative measurement of vitamin K2 (menaquinones) in various fermented dairy products using a reliable high-performance liquid chromatography methodJ Dairy Sci.(2013 Mar)
- ^Kamao M, Suhara Y, Tsugawa N, Uwano M, Yamaguchi N, Uenishi K, Ishida H, Sasaki S, Okano TVitamin K content of foods and dietary vitamin K intake in Japanese young womenJ Nutr Sci Vitaminol (Tokyo).(2007 Dec)
- ^Elder SJ, Haytowitz DB, Howe J, Peterson JW, Booth SLVitamin k contents of meat, dairy, and fast food in the u.s. DietJ Agric Food Chem.(2006 Jan 25)
- ^Shimogawara K, Muto SPurification of Chlamydomonas 28-kDa ubiquitinated protein and its identification as ubiquitinated histone H2BArch Biochem Biophys.(1992 Apr)
- ^Hirauchi K, Sakano T, Notsumoto S, Nagaoka T, Morimoto A, Fujimoto K, Masuda S, Suzuki YMeasurement of K vitamins in animal tissues by high-performance liquid chromatography with fluorimetric detectionJ Chromatogr.(1989 Dec 29)
- ^Chen GC, Wang Y, Tong X, Szeto IMY, Smit G, Li ZN, Qin LQCheese consumption and risk of cardiovascular disease: a meta-analysis of prospective studiesEur J Nutr.(2017 Dec)
- ^Villines TC, Hatzigeorgiou C, Feuerstein IM, O'Malley PG, Taylor AJVitamin K1 intake and coronary calcificationCoron Artery Dis.(2005 May)
- ^Hao G, Zhang B, Gu M, Chen C, Zhang Q, Zhang G, Cao XVitamin K intake and the risk of fractures: A meta-analysisMedicine (Baltimore).(2017 Apr)
Examine Database References
- Bone Mineral Density - Braam LA, Knapen MH, Geusens P, Brouns F, Hamulyák K, Gerichhausen MJ, Vermeer CVitamin K1 supplementation retards bone loss in postmenopausal women between 50 and 60 years of ageCalcif Tissue Int.(2003 Jul)
- Bone Mineral Density - Purwosunu Y, Muharram, Rachman IA, Reksoprodjo S, Sekizawa AVitamin K2 treatment for postmenopausal osteoporosis in IndonesiaJ Obstet Gynaecol Res.(2006 Apr)
- Bone Mineral Density - Sasaki N, Kusano E, Takahashi H, Ando Y, Yano K, Tsuda E, Asano YVitamin K2 inhibits glucocorticoid-induced bone loss partly by preventing the reduction of osteoprotegerin (OPG)J Bone Miner Metab.(2005)
- Bone Mineral Density - Forli L, Bollerslev J, Simonsen S, Isaksen GA, Kvamsdal KE, Godang K, Gadeholt G, Pripp AH, Bjortuft ODietary vitamin K2 supplement improves bone status after lung and heart transplantationTransplantation.(2010 Feb 27)
- Bone Mineral Density - Shiraki M, Shiraki Y, Aoki C, Miura MVitamin K2 (menatetrenone) effectively prevents fractures and sustains lumbar bone mineral density in osteoporosisJ Bone Miner Res.(2000 Mar)
- Estrogen - Ozuru R, Sugimoto T, Yamaguchi T, Chihara KTime-dependent effects of vitamin K2 (menatetrenone) on bone metabolism in postmenopausal womenEndocr J.(2002 Jun)
- Bone Mineral Density - Marissa M Shams-White, Mei Chung, Zhuxuan Fu, Karl L Insogna, Micaela C Karlsen, Meryl S LeBoff, Sue A Shapses, Joachim Sackey, Jian Shi, Taylor C Wallace, Connie M WeaverAnimal Versus Plant Protein and Adult Bone Health: A Systematic Review and Meta-Analysis From the National Osteoporosis FoundationPLoS One.(2018 Feb 23)
- Bone Mineral Density - Min-Yu Tu, Hsiao-Ling Chen, Yu-Tang Tung, Chao-Chih Kao, Fu-Chang Hu, Chuan-Mu ChenShort-Term Effects of Kefir-Fermented Milk Consumption on Bone Mineral Density and Bone Metabolism in a Randomized Clinical Trial of Osteoporotic PatientsPLoS One.(2015 Dec 10)
- Bone Mineral Density - Shi S, Wang F, Huang Y, Chen B, Pei C, Huang D, Wang X, Wang Y, Kou S, Li W, Ma T, Wu Y, Wang ZEpimedium for Osteoporosis Based on Western and Eastern Medicine: An Updated Systematic Review and Meta-Analysis.Front Pharmacol.(2022)
- Fracture Risk - Bischoff-Ferrari HA, Willett WC, Wong JB, Stuck AE, Staehelin HB, Orav EJ, Thoma A, Kiel DP, Henschkowski JPrevention of nonvertebral fractures with oral vitamin D and dose dependency: a meta-analysis of randomized controlled trialsArch Intern Med.(2009 Mar 23)
- Interleukin 6 - Mozaffari-Khosravi H, Hesabgar HA, Owlia MB, Hadinedoushan H, Barzegar K, Fllahzadeh MHThe effect of garlic tablet on pro-inflammatory cytokines in postmenopausal osteoporotic women: a randomized controlled clinical trialJ Diet Suppl.(2012 Dec)